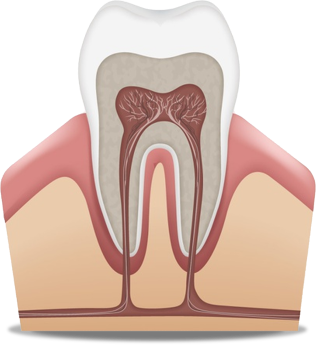
Impacted teeth are a common dental anomaly where a tooth either fails to fully erupt from the gum or remains partially or completely hidden beneath the gingival tissue. Impacted canine teeth and wisdom teeth (third molars) are the most frequently observed types. These impactions can occur in various forms, resting horizontally or vertically within the jawbone or under the gum.
Causes and Treatment of Impacted Teeth
Canine impaction has various causes that differ from person to person. An impacted tooth may become trapped within the gum for different reasons, such as lack of sufficient space.
Impacted canine anomalies are classified into different positions within the mouth, and each type is guided to its correct position using a specific treatment method. Unlike wisdom teeth, which are usually extracted when impacted or partially impacted, extraction is typically not the preferred method for an impacted canine. Instead, the dentist decides on the treatment based on the angle of impaction, the patient’s age, and the type of impaction.
Treating Impacted Canines
Sometimes, obstacles preventing the eruption of the impacted tooth can be resolved simply by removing a small section of gum tissue. Other times, extracting a persistent baby tooth that is blocking the permanent canine can create the necessary space for it to erupt. When treating an impacted tooth, the angle of impaction and the patient’s age must be considered.
For cases where the anomaly is not severe, orthodontics is a recommended treatment. In more severe cases, a surgical approach must be used to expose a portion of the tooth’s crown so it can be guided into position using orthodontic appliances.
Specifically, the patient first visits a dental clinic where an orthodontist diagnoses the type of canine impaction. Then, the orthodontist uses orthodontic methods to create the necessary space for the canine to erupt. Following this, the patient visits a surgeon, who performs a minor surgery to expose the tooth by removing a section of the gum.
Finally, using the orthodontic method, the impacted tooth is put on its path of treatment and guided to its correct location. The impacted tooth is moved out of the gum by applying force generated through the orthodontic appliances. In this procedure, the amount of tooth movement is approximately one to three millimeters per month until it reaches its natural position in the dental arch.
Types of Impacted Teeth: Labial and Palatal Impaction
Impacted teeth, especially canines, are classified based on the direction of their displacement:
Labial Impaction: This is a type of canine impaction where the tooth shifts toward the cheek or lip side (labial/buccal). A lack of adequate space in the jaw prevents the tooth from emerging from the gum.
Palatal Impaction: In palatal canine impaction, the tooth is displaced toward the roof of the mouth (palate). This deviation from the normal dental path prevents the tooth from erupting.
Consequences of Untreated Impacted Canines
The canine tooth is a key, highly functional tooth, and if its impaction is not properly treated, it can lead to serious problems and potential pathology. The following issues may result from an untreated impacted canine:
Infection: If the tooth remains impacted, bacteria and inflammatory tissues can accumulate beneath it, causing pain and gum swelling. Occasionally, the infection may spread to other parts of the body, leading to more serious systemic conditions.
Changes in Tooth Position: An impacted canine can cause other teeth to shift in position. This positional change may lead to crowding, fracturing of adjacent teeth, the creation of gaps between teeth, or misalignment of the bite (malocclusion) between the upper and lower jaws.
Inflammation: The condition of an impacted canine trapped within the gum tissue can cause localized inflammation. If left untreated, this inflammation can progress to outright infection or intensify the existing inflammatory state.
Jaw Disorders: Sometimes, a canine impaction can be associated with temporomandibular joint (TMJ) disorders or jaw pain. For the patient, this may manifest as pain, jaw stiffness, difficulty chewing, or even contribute to breathing problems.
Abrasion/Wear: In some instances, an impacted canine may attempt to erupt or interfere with the roots or crowns of other teeth. This interference can cause abrasion, scratching, or decay of adjacent, healthy teeth.
Cysts and Tumors: Beyond damaging the health of adjacent teeth and diminishing the aesthetics of the smile, an impacted canine may—depending on the patient’s age—lead to the development of cysts and tumors in the affected jaw area. The presence of any impacted tooth, combined with advanced patient age and reduced jaw elasticity, increases the risk of developing jaw cysts and tumors.
Damage to Roots of Adjacent Teeth: An impacted tooth can cause damage to the roots of nearby teeth, potentially leading to their resorption or loss.
Premature Wear of Other Teeth: The presence of the impacted tooth and its resulting misalignment can lead to excessive and premature wear on other teeth in the mouth.
Other Ailments: Occasionally, the presence of an impacted tooth may be linked to other health issues such as dizziness (vertigo) and chronic headaches.

Wisdom Teeth
Wisdom teeth (third molars) typically begin developing around the age of nine and naturally erupt from the jawbone between the ages of 17 and 25. If there is insufficient space for the wisdom tooth to erupt, it can become impacted in the gum tissue. This often leads to severe pain, extensive infections, and general oral health problems for the patient. In such situations, the wisdom tooth must be removed, either through simple extraction or surgery.
Dentists usually recommend the removal or surgical extraction of an impacted wisdom tooth because of the problems it can cause. Common reasons for wisdom tooth removal include:
Impaction: The tooth gets stuck beneath the gum line due to lack of space.
Abnormal Eruption: The wisdom tooth emerges from the gum in an unnatural position (tilted, rotated, angled, etc.).
Bite Change: The eruption causes a shift in how the upper and lower teeth meet, leading to misalignment of the jaws.
Infection: Food particles, plaque, and bacteria get trapped around the wisdom tooth, causing infection (pericoronitis).
Rapid Decay: The wisdom tooth quickly develops cavities because its position makes it difficult to reach and maintain proper hygiene.
Classification of Impacted Wisdom Tooth Depth
The depth of the impacted wisdom tooth (third molar) relative to the occlusal plane (the chewing surface) is classified as follows:
Class A: In this position, the tooth is not trapped within the bone and is level with the adjacent tooth’s chewing surface.
Class B: Occurs when the cemento-enamel junction (CEJ) of the impacted tooth is below the level of the adjacent tooth’s chewing surface, but not entirely submerged.
Class C: A condition where the tooth is completely hidden within the bone, and the impacted tooth’s occlusal plane is below the cervical line (neck) of the adjacent tooth.
Impaction is also classified based on the tooth’s relationship to the anterior border of the ramus (the ascending part of the jawbone):
Class 1: The tooth is entirely anterior to the anterior border of the mandibular ramus.
Class 2: Half of the tooth’s crown is covered by the anterior border of the ramus.
Class 3: The entire crown of the tooth is covered by the anterior border of the ramus.
When is Surgical Removal of an Impacted Wisdom Tooth Necessary?
Surgical removal of an impacted wisdom tooth is mandatory and recommended by the dentist in the following situations:
Damage to Other Teeth: When the wisdom tooth is pressing against or causing resorption or decay in adjacent teeth.
Severe Pain: Persistent and intense pain that cannot be managed with medication.
Gum Infection: Recurrent or severe infection of the gum tissue surrounding the impacted tooth (pericoronitis).
Bone Infection: Spread of infection into the jawbone (osteomyelitis).
Systemic Infection: When the local infection spreads to other parts of the body, causing systemic symptoms such as fever, swelling, extreme fatigue, body aches, etc.
The Surgical Process for Impacted Wisdom Tooth Removal
The standard procedure for extracting an impacted wisdom tooth involves the following stages:
Examination and Consultation: The dentist assesses the tooth’s position, discusses the procedure, and plans the removal.
Anesthesia/Sedation: The area is numbed using local anesthesia or the patient is given sedation for comfort.
Impacted Wisdom Tooth Extraction/Surgery: The tooth is surgically removed.
Essential Post-Operative Care After Impacted Wisdom Tooth Surgery
Following the surgical removal of a wisdom tooth, specific care instructions must be followed to ensure proper healing and prevent complications:
Maintain Pressure on Gauze: Keep the sterile gauze firmly pressed on the surgical site for at least one hour.
Avoid Frequent Gauze Changes: Do not quickly change the gauze at the operative site, as premature removal can interfere with the formation of the blood clot (which is essential for healing).
Refrain from Forceful Mouth Rinsing or Spitting: Avoid aggressive rinsing or spitting for at least 24 hours after the surgery.
Drink from a Glass: Drink liquids directly from a glass; do not use a straw, as the suction can dislodge the blood clot.
Rinse with Salt Water: Begin gently rinsing your mouth with a dilute salt water solution only after the first 24 hours have passed.
Rest and Limit Activity: Ensure you get sufficient rest and avoid strenuous physical activity.
Avoid Hot Foods/Drinks: Do not consume hot beverages or food for the remainder of the surgery day.
Complications of Wisdom Tooth Surgery
The natural, expected complications following this type of surgery include facial swelling, pain, jaw stiffness (trismus), minor bleeding, and discomfort. Other potential complications include:
Infection: Developing an infection at the surgical site.
Damage During Surgery: Injury to the jawbone or adjacent teeth during the extraction process.
Severe Pain from Dry Socket: Intense pain resulting from a condition called Alveolar Osteitis (Dry Socket), which occurs when the protective blood clot is lost.
Nerve Injury: Numbness of the lower lip or tongue (paresthesia) and persistent jaw stiffness.
For accessing the most appropriate and high-quality dental services and minimizing potential side effects, consultation with an experienced specialist is highly recommended. Dr. Abdolsafa Sherafati specialized clinic, with its wealth of experience and expert consultation, is dedicated to assisting patients in achieving the best possible clinical outcomes.